What Causes Tendinopathy and How Can It Be Treated?
The terminology to describe tendinitis has changed over the last ten years or so to Tendinopathy due to a lack of evidence that it is an inflammatory condition. Any medical term with “itis” as a suffix is defined as inflammatory in nature so therefore tendinitis is an outdated term.
Although initially, it is reasonable to conclude that there is an element of inflammation at the site of microtrauma, progression of such conditions have been consistently demonstrated to have no long term inflammatory qualities.
Incidence of tendinopathy is increasing in the developed world due to increased participation in recreational sport. However, it is not only sports enthusiasts that develop tendinopathy as it has links to other overuse and/or repetitive load with work related activities. Also, several metabolic disorders have been identified as underlying factors in tendinopathy and obesity, hypertension, diabetes mellitus, hypercholesterolemia, and other metabolic illnesses have been clearly associated with increased incidence of tendinopathy.
The collagen in normal tendon tissue is very uniform in structure. Tendinosis is the process of increased collagen being laid down a disorganised manner on tendon tissue in response to potential overload of the muscle that ultimately can develop into a tendinopathy.
The basic progression is that after exercise, normal processes induce protein breakdown of tendon tissue. This is followed by increased synthesis of collagen to repair exercise induced microtrauma in the tissues. There is a required rest period between bouts of exercise to balance the tissue repair. If that rest period is not observed then there is a net collagen gain, leading over time a thickening of the tendon itself.
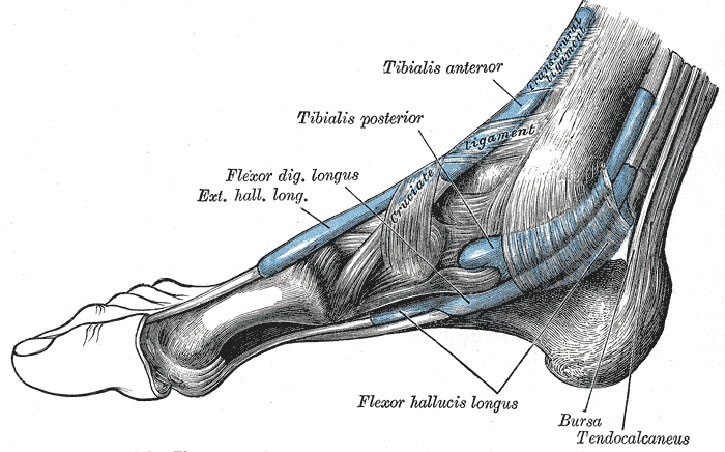
A secondary factor is increased vascularity in the tendon itself. Healthy tendon is mostly avascular (no specific blood supply) and aneuronal ( no specific nerve supply). Where blood vessels go, nerves will follow so tendon tissue gains the ability to be painful. It is thought that repetitive micro-trauma initiates the increase in vascular and neural tissue infiltrating the tendon. Initially what may be inflammatory discomfort following exercise, over time becomes more chronic as the tissue changes take place and no longer require inflammatory processes to be felt as sore or painful.
There have been many treatments tried over the years, with some positive results on certain types of tendinopathy ( or at different anatomical positions). Successful conservative treatments include eccentric exercise, which loads and lengthens the muscle of the affected tendon. One recent study of 200 patients given a 6 week protocol of eccentric exercise had 44% of subjects report complete resolution while another 43% reporting significant improvement.
Tissue injection material such as corticosteroids are proving controversial as although there have been short term improvements demonstrated, long term outcomes are now showing a negative effect.
One positive injective material although it has not been used for long enough to gather long term outcome, is Platelet Rich Plasma, known as PRP. This is where blood is taken from the patient and put in a centrifuge to separate the red blood cells from the clear but cloudy plasma. The plasma is then re-injected back into the tendon tissue directly.
Extracorporeal shockwave treatment and low-intensity pulsed ultrasound, initiate tendon and tendon-to-bone healing. Thus, shockwave and ultrasound have both demonstrated positive experimental effects on tendon healing; Shockwave selectively denervates sensory nerve fibres without disturbing larger motor neurons.
Exercising with a tendinopathy is generally considered to be completely safe but advice should be sought as to what is appropriate. Movement creates heat which makes the tendon tissue more pliable and pain will generally reduce during exercise while symptoms will be at their worst at times of rest or moving after rest. A typical daily pattern for Achilles tendinopathy shows pain and dysfunction to be at its worst in the morning when standing from the bed.
Pain can be helped with ibuprofen, which although an anti-inflammatory medication has been shown to help. However not all anti-inflammatories help as Naproxen, another, stronger anti-inflammatory, has not been shown to help in the majority of patients.
Icing the area can help with pain, although it is used for managing symptoms only. Neither anti-inflammatories or Ice will help with improvement to the tissues.
Tendinopathy has been demonstrated to be a chronic condition, however, there is plenty of evidence that these type of issues are treatable and that patients can lead perfectly normal, fit and healthy lifestyles by making some changes to factors that generated the mechanism of onset and with some specific treatment options.
For more information, or to book a sports injury consultation, please call The Body Matters on01702 714 968.
- Understanding Amnanda: A Gentle Path Back to Balance - 19th December 2025
- How Amnanda Can Help with Headaches - 27th November 2025
- Rest and Realign: Coming Home to the Body - 27th October 2025
